ADHD, iPads, sleep and concentration problems: Shedding new light on ADHD?
July 1, 2018 - neurocare group
In classrooms, the idea still prevails that easily distracted children and children with ADHD should not be seated too close to the window since they might be distracted by what is happening outside. ADHD is also often associated with difficulties in executive functioning and attention. Are these symptoms truly the core issue of ADHD? Or could there be a different underlying cause? In this article, we will explain how some easily distracted children might be better off sitting closer to the window given the connection between ADHD and sunlight.
Most parents are aware that no two children are the same. Accordingly, we know that no two children with ADHD are the same, even though they share the same broad “diagnosis”. It is strange that even in psychiatry this principle has only been recently accepted.
In recent years it has become more evident that the treatment of ADHD with psychostimulant medications have only sustained effects beyond 2 years in 30-40% of patients. This observation indicates that we should accept the possibility of more than one cause for ADHD and that – from a neurobiological perspective – it is not a homogeneous disorder. This notion has lead to a development in “personalized medicine” or “Precision Medicine”, whereby a range of therapeutic approaches is needed to treat the diversity of ADHD “behaviours”.
Since 2001neurocare in The Netherlands (now in Australia, the US and Germany) has conducted research on certain ADHD subgroups. These studies found that children with brain activity indicating drowsiness respond well to both psychostimulant medication and also neurofeedback. Conceptually, it is also very understandable that a psychostimulant medicine should have an effect when there are signs of drowsiness. It should be noted, however, that there are some parties ‘over-claiming’ the efficacy of Neurofeedback as a treatment for various other disorders.
An online search of the term “Neurofeedback” often leads us to think this is a new treatment approach for a range of mental or cognitive issues. It should also be noted that a wide variety of “Neurofeedback methods” have been applied, of which some are well-investigated and known to have good clinical effects, whereas many others have more questionable methods which have not been investigated at all.
For this reason, we advise people to look for therapists who claim less of their treatment services (e.g., who limit themselves to the treatment of ADHD). And, just like regular ADHD treatment should be carried out by a trained psychologist, the same should apply to neurofeedback treatment. In working with neurofeedback and ADHD, we have noticed for years that the most common “side-effect” reported by patients, was that they slept better, even when no sleeping problems were present. Based on this fact and other scientific studies explaining this “sleep enhancing effect” of neurofeedback, we recently published a model that relates sleep problems to symptoms in the ADHD spectrum, such as concentration problems, impulsivity, etc. (Arns & Kenemans, 2012.)
What is the connection between sleep problems and ‘symptoms of ADHD’
Figure 1: In the blue map of this illustration the prevalence of ADHD across various US states can be seen, where especially in the south-west lower prevalence of ADHD are found (light blue: CDC 2003). The colored map represents the intensity of sunlight in KWh/m2/dag: NREL). This video illustrates the clear overlap between high sunlight intensity (red areas) and low ADHD prevalence (light blue areas), where a high sunlight intensity seems protective of against the development of ADHD. To replay the movie, press the ‘play’ button again.
How understanding the effects of Blue Light can help prevent ADHD
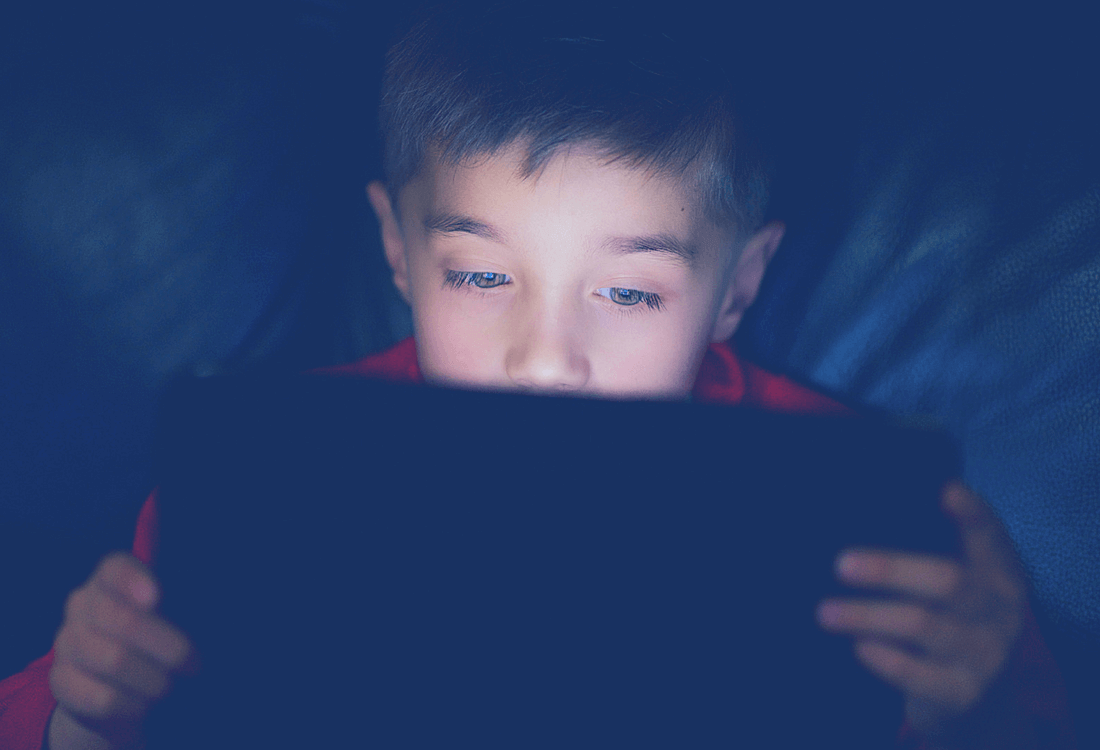
Now, of course, the question arises whether it is recommendable to keep children from using the iPad or computer in the evening. Our research shows that sufficient exposure to sunlight during the day may have a preventative effect in ADHD. However, it is our interpretation that this is caused by an excessive amount of blue light exposure in the evening. Banning modern media use in the evening will probably not be realistic. However, free software is available (like F.lux) that will adjust the colour settings on the screen of your PC, Mac or iPad, depending on the time of day. Manufacturers of modern media should perhaps consider implementing this functionality by default, such as the ‘Night Shift’ feature recently implemented by Apple for iOS devices such as iPhones and iPads. Also, LED manufacturers may consider developing LED lights with less affinity in the blue spectrum. Yet, a simple advice may be to just get more daylight exposure in the morning. A project of which we are still dreaming is to literally ‘take the roof off’ in schools in the Netherlands, in order to use skylight to provide natural light in the classrooms. The only ‘side effect’ of such an intervention would be substantial savings on energy costs, thus an ecologically sustainable solution, and possibly a decrease in concentration problems and ADHD. Until that time, simple advice like walking the dog in the morning, walking or cycling to school instead of using a car and, as argued above, providing a seat by the window for that easily distracted child, are a good start.